Inflammation: The Missing Link Between Cardiometabolic, Immunologic, and Neurodegenerative Diseases
Have you ever wondered why patients affected by obesity or other cardiometabolic conditions often suffer from a multitude of seemingly unrelated diseases, like psoriasis or Alzheimer’s disease? Recent research has uncovered commonalities within the pathologies behind these conditions that implicate chronic inflammation as a major driver of disease development and progression. This article summarizes the current research landscape of how inflammation is thought to contribute to the cooccurrence of seemingly unconnected diseases and their widespread impact on the global population.

Inflammation is a transient evolutionary process whose role is to respond to injury or infection.1-4 However, under certain conditions, systemic, low-grade, chronic inflammation develops, resulting in damage to tissues or organs over time.1 Chronic inflammation has been implicated in a variety of cardiometabolic disorders such as type 2 diabetes, obesity, metabolic dysfunction–associated steatohepatitis (MASH), hypertension, and cardiovascular disease (CVD).1,4–8 Although the exact molecular mechanisms underlying chronic inflammation and the development of these disorders are yet to be fully elucidated,9 experts agree that inflammation can be both a cause and a consequence of various cardiometabolic diseases.3
Atherosclerosis (ACS), a chronic inflammatory disease associated with impaired metabolism, develops when low-density lipoprotein cholesterol accumulates in the endothelium of arteries, triggering an inflammatory response and plaque formation. Elevated circulating inflammatory markers such as C-reactive protein, serum amyloid A, interleukin (IL)-6, and IL-1 receptor antagonist commonly accompany ACS and independently correlate with in-hospital and short-term adverse prognoses.3,10-12
In type 2 diabetes, another cardiometabolic condition, elevated blood glucose induces oxidative stress that leads to chronic inflammation. This hyperglycemic state promotes the formation of advanced glycation end products, which bind to certain proteins and enhance the production of proinflammatory cytokines. Persistent inflammation results in insulin resistance that further exacerbates high glucose levels.3,11,13,14
In obesity, expanded adipose tissue releases cytokines and adipokines that promote a proinflammatory environment. Macrophage release of cytokines, tumor necrosis factor (TNF)-α, and IL-6 contributes to glucose disruptions and insulin resistance. Adipokine leptin participates in the regulation of innate and adaptive immune responses and elevates cytokine levels (Figure 1).3,7,11,15

Figure 1. Mechanisms of chronic inflammation in obesity.4,6,15–22
The inflammatory environments promoted by cardiometabolic diseases may increase risk or compound the severity of other conditions associated with chronic inflammation, as seen in some neurodegenerative and immunologic diseases.1 This interplay is seen in Alzheimer’s disease, a progressive neurodegenerative disorder that affects 27 million people worldwide and corresponds to 60%–70% of all dementia cases.23,24 Current research suggests that this neurodegenerative condition develops through the aggregation of amyloid β into fibrils, the formation of extracellular tangles by hyperphosphorylation of tau protein, and chronic neuroinflammation.15,19,24 The association between Alzheimer’s disease and inflammation-promoting cardiometabolic illnesses is corroborated by the observations that patients with obesity have an almost 2-fold higher risk of developing this disorder.25 Moreover, “type 3 diabetes” has been suggested as a name for Alzheimer’s disease because of its link to type 2 diabetes.19
Psoriasis is a chronic, inflammatory disease that affects 125 million people globally.9 This autoimmune disorder, along with other skin diseases such as atopic dermatitis and hidradenitis suppurativa, are associated with the occurrence of obesity, and their risk increases with high abdominal fat as well as weight gain.26–33 Psoriasis has also been linked to other inflammatory cardiometabolic disorders such as type 2 diabetes and CVD.26,34,35 The pathophysiology of this autoimmune disease includes stimulation of immune cells, leading to increased generation of proinflammatory cytokines and immune-modulating activity of adipokines.26,31,34
Atopic dermatitis, also known as atopic eczema, is a chronic, recurrent, inflammatory disease that affects 171 million individuals worldwide.20,36–38 The pathophysiology of atopic dermatitis is multifactorial and involves skin barrier impairment through cytokine-stimulated immune response.38 As with psoriasis, research on atopic dermatitis has demonstrated associations with cardiovascular and metabolic diseases.39 Together, the cardiometabolic, neurodegenerative, and immunologic diseases discussed above affect millions of people globally (Figure 2). Therefore, it is crucial to expand our understanding of the components and intricate mechanisms involved in the generation of these conditions.
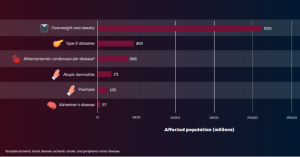
Figure 2. Global impact of diseases linked to chronic inflammation.9,24,29,37,40–42
Chronic inflammation appears to be a connection shared by multiple cardiometabolic, neurodegenerative, and immunologic disorders. Evolving insights into the role of inflammation in pathophysiology across disease states have opened important new areas of clinical research, including the potential to use inflammatory biomarkers for disease risk stratification and monitoring treatment response.11 Because it is possible that there are joint pathophysiological mechanisms underlying these conditions, therapies that target shared inflammatory pathways may be beneficial to patients.
In our next article, we will focus on rapidly evolving novel treatment options – ie, incretins – that are poised to become a potential solution for targeting systemic diseases connected by common, yet not fully understood, molecular pathways.
References
- Furman D, Campisi J, Verdin E, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25(12):1822-1832.
- Lee YS, Jun HS. Anti-Inflammatory effects of GLP-1-based therapies beyond glucose control. Mediators Inflamm. 2016;2016:3094642.
- Tate AR, Rao GHR. Inflammation: is it a healer, confounder, or a promoter of cardiometabolic risks? Biomolecules. 2024;14(8):948.
- Ruck L, Wiegand S, Kühnen P. Relevance and consequence of chronic inflammation for obesity development. Mol Cell Pediatr. 2023;10(1):16.
- Donath MY, Meier DT, Böni-Schnetzler M. Inflammation in the pathophysiology and therapy of cardiometabolic disease. Endocr Rev. 2019;40(4):1080-1091.
- Manabe I. Chronic inflammation links cardiovascular, metabolic and renal diseases. Circ J. 2011;75(12):2739-2748.
- Ruppert Z, Neuperger P, Rákóczi B, et al. Characterization of obesity-related diseases and inflammation using single cell immunophenotyping in two different diet-induced obesity models. Int J Obes (Lond). 2024;48(11):1568-1576.
- Hunter P. The inflammation theory of disease. The growing realization that chronic inflammation is crucial in many diseases opens new avenues for treatment. EMBO Rep. 2012;13(11):968-970.
- Aksentijevich M, Lateef SS, Anzenberg P, Dey AK, Mehta NN. Chronic inflammation, cardiometabolic diseases and effects of treatment: psoriasis as a human model. Trends Cardiovasc Med. 2020;30(8):472-478.
- Liu M, Chen R, Zheng Z, et al. Mechanisms of inflammatory microenvironment formation in cardiometabolic diseases: molecular and cellular perspectives. Front Cardiovasc Med. 2025;11:1529903.
- Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105(9):1135-1143.
- Neeland IJ, Ross R, Després JP, et al; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019;7(9):715-725.
- Weinberg Sibony R, Segev O, Dor S, Raz I. Overview of oxidative stress and inflammation in diabetes. J Diabetes. 2024;16(10):e70014.
- Xu B, Wu Q, La R, et al. Is systemic inflammation a missing link between cardiometabolic index with mortality? Evidence from a large population-based study. Cardiovasc Diabetol. 2024;23(1):212.
- Christensen A, Pike CJ. Menopause, obesity and inflammation: interactive risk factors for Alzheimer’s disease. Front Aging Neurosci. 2015;7:130.
- Castanon N, Lasselin J, Capuron L. Neuropsychiatric comorbidity in obesity: role of inflammatory processes. Front Endocrinol (Lausanne). 2014;5:74.
- Kwiat VR, Reis G, Valera IC, Parvatiyar K, Parvatiyar MS. Autoimmunity as a sequela to obesity and systemic inflammation. Front Physiol. 2022;13:887702.
- Park CS, Shastri N. The role of T cells in obesity-associated inflammation and metabolic disease. Immune Netw. 2022;22(1):e13.
- Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55(1):31-55.
- Guo Z, Yang Y, Liao Y, Shi Y, Zhang LJ. Emerging roles of adipose tissue in the pathogenesis of psoriasis and atopic dermatitis in obesity. JID Innov. 2021;2(1):100064.
- Oleinika K, Slisere B, Catalán D, Rosser EC. B cell contribution to immunometabolic dysfunction and impaired immune responses in obesity. Clin Exp Immunol. 2022;210(3):263-272.
- Kosyreva AM, Sentyabreva AV, Tsvetkov IS, Makarova OV. Alzheimer’s disease and Inflammaging. Brain Sci. 2022;12(9):1237.
- Scheltens P, De Strooper B, Kivipelto M, et al. Alzheimer’s disease. Lancet. 2021;397(10284):1577-1590.
- Silva MVF, Loures CMG, Alves LCV, de Souza LC, Borges KBG, Carvalho MDG. Alzheimer’s disease: risk factors and potentially protective measures. J Biomed Sci. 2019;26(1):33.
- Picone P, Di Carlo M, Nuzzo D. Obesity and Alzheimer’s disease: molecular bases. Eur J Neurosci. 2020;52(8):3944-3950.
- Jensen P, Skov L. Psoriasis and obesity. Dermatology. 2016;232(6):633-639.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76(3):377-390.
- Palanivel JA, Millington GWM. Obesity-induced immunological effects on the skin. Skin Health Dis. 2023;3(3):e160.
- Li X, Zhu J, Zhao W, et al. The causal effect of obesity on the risk of 15 autoimmune diseases: a Mendelian randomization study. Obes Facts. 2023;16(6):598-605.
- Yamazaki F. Psoriasis: comorbidities. J Dermatol. 2021;48(6):732-740.
- Darlenski R, Mihaylova V, Handjieva-Darlenska T. The link between obesity and the skin. Front Nutr. 2022;9:855573.
- Petrasca A, Hambly R, Kearney N, et al. Metformin has anti-inflammatory effects and induces immunometabolic reprogramming via multiple mechanisms in hidradenitis suppurativa. Br J Dermatol. 2023;189(6):730-740.
- Sivanand A, Gulliver WP, Josan CK, Alhusayen R, Fleming PJ. Weight loss and dietary interventions for hidradenitis suppurativa: a systematic review. J Cutan Med Surg. 2020;24(1):64-72.
- Paschou IA, Sali E, Paschou SA, Psaltopoulou T, Nicolaidou E, Stratigos AJ. The effects of GLP-1RA on inflammatory skin diseases: a comprehensive review. J Eur Acad Dermatol Venereol. Published online April 29, 2025.
- Piaserico S, Orlando G, Messina F. Psoriasis and cardiometabolic diseases: shared genetic and molecular pathways. Int J Mol Sci. 2022;23(16):9063.
- Schuler CF 4th, Billi AC, Maverakis E, Tsoi LC, Gudjonsson JE. Novel insights into atopic dermatitis. J Allergy Clin Immunol. 2023;151(5):1145-1154.
- Faye O, Flohr C, Kabashima K, et al. Atopic dermatitis: a global health perspective. J Eur Acad Dermatol Venereol. 2024;38(5):801-811.
- Frazier W, Bhardwaj N. Atopic dermatitis: diagnosis and treatment. Am Fam Physician. 2020 May 15;101(10):590-598.
- Untaaveesup S, Amnartpanich T, Jirattikanwong N, et al. Cardiovascular and metabolic outcomes associated with moderate-to-severe atopic dermatitis: a systematic review and meta-analysis. World Allergy Organ J. 2025;18(3):101035.
- GBD 2021 Adult BMI Collaborators. Global, regional, and national prevalence of adult overweight and obesity, 1990-2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. Lancet. 2025 Mar 8;405(10481):813-838.
- Li Z, Yang Y, Wang X, et al. Comparative analysis of atherosclerotic cardiovascular disease burden between ages 20-54 and over 55 years: insights from the Global Burden of Disease Study 2019. BMC Med. 2024 Jul 19;22(1):303.
- Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes: global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107-111.
Share